Terminally-ill bowel cancer patient sues over delayed diagnosis, missed opportunities for treatment
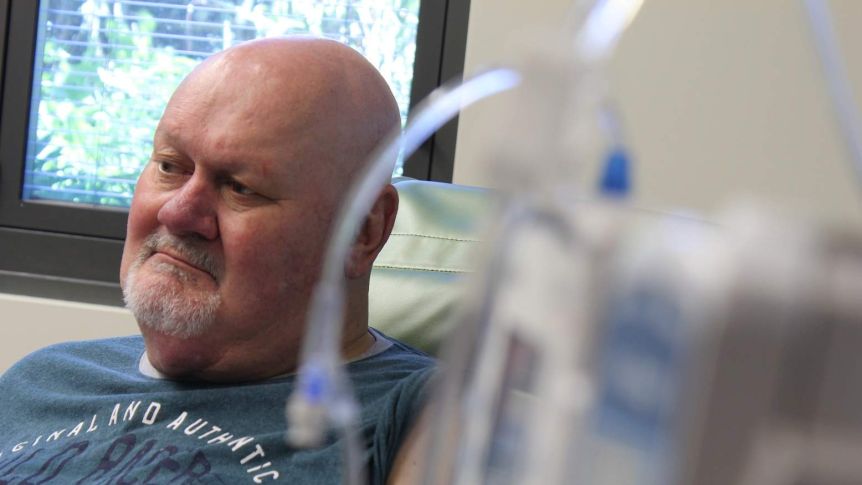
A 58-year-old man is taking his former GP and hospital to court claiming they failed to detect a cancerous tumour in time to stop it becoming terminal.
Key points:
- A court claim argues Jeff Whitehead’s treatment was negligent and reduced his life expectancy
- Mr Whitehead said his GP dismissed his positive bowel screening test result
- In defences lodged with the court, the hospital and GP both deny their actions were negligent
Jeff Whitehead was rushed to hospital for urgent surgery in June 2018 after a CT scan revealed a tumour the size of a cricket ball in the junction between his large and small intestines.
“The tumour had broken out of my bowel and [the doctor] said it was like an octopus trying to latch onto the inside of my stomach,” he said.
“It ended up going to my liver and lungs.”
Mr Whitehead was living alone in Maryborough, north-west of Melbourne, at the time, and had been suffering worsening symptoms including abdominal pain, constipation, and weight loss for months.
He said, at multiple points, his symptoms were not properly investigated and he now has fewer than 12 months to live.
“The cost is my life, that’s what it is, and I can’t get that back,” he said.
“More should have been done earlier.”

‘Multiple missed opportunities’
A statement of claim on behalf of Mr Whitehead has been lodged, alleging his treatment from both the Maryborough District Health Service and his former GP were negligent.
The document, lodged with the court in October, argues the alleged negligence had resulted in “injury, loss and damage”, including the “progression of caecal adenocarcinoma, metastatic spread of adenocarcinoma, and reduced life expectancy”.
“There is a difference between unlucky, and perhaps negligent, circumstances,” Mr Whitehead’s lawyer, Alice Robinson, said.
“We now know with the expert evidence we’ve gathered that he’s suffering from something which is more likely than not preventable, and avoidable.
“Between his GP and the hospital, there were multiple missed opportunities for treatment which would have made a big difference to Jeff’s health now,” Ms Robinson said.
Find more local news
Mr Whitehead first went to see his doctor complaining of abdominal symptoms in May 2017.
By August of that year, his doctor had organised a colonoscopy, a procedure that looks for abnormalities in the bowel.
The result came back normal, but Mr Whitehead said his symptoms began to get worse and he was inexplicably losing weight.
Mr Whitehead’s lawyer argued that “reasonable medical practice” on the part of the hospital would have identified his tumour, and had it been identified his chances of survival would have improved.
Ms Robinson also claimed that Mr Whitehead’s GP failed in his duty of care to properly investigate his patient’s symptoms when the colonoscopy failed to provide a diagnosis.
In separate defences lodged with the court, both the hospital and Mr Whitehead’s GP have denied their actions were negligent.
Patient told ‘you don’t have cancer’
Part of the claim centres around the GP’s response to a positive result that Mr Whitehead received from the national bowel screening test in February 2018.
Mr Whitehead said he took the test after it came in the post and then made an appointment with his GP when it came back positive.
“He looked at me before I sat down and said ‘what’d you to do that for?’
“And I said ‘because it came in the mail and it’s a positive’.
“He didn’t even open it. He just screwed it up, the envelope with the letter in it, and threw it in his waste-paper bin.
“And he said ‘how many times I’ve got to tell you, you don’t have cancer’.”
Medical records viewed by the ABC reveal the doctor did not recommend further investigation of the result at the time.

It was only by chance that another doctor picked up there was a serious problem after routine blood tests were taken in the lead-up to a knee operation the same month.
The results found several red flags including iron deficiency and the presence of a protein that can be linked to cancer.
Mr Whitehead’s GP became aware of the February blood test results in March. It was another three months before he ordered the CT scan which revealed the large tumour in his patient’s bowel.
By that stage, the cancer had spread to other parts of his body.
In a defence filed to the Supreme Court, lawyers for the doctor have admitted he did not suggest further investigation of the positive bowel screening test, stating that “the colonoscopy and subsequent histopathology was reported as revealing no abnormality”.
Clinical guidelines for general practitioners from the time state, once a decision is made to investigate, “if investigations are incomplete, an alternative investigation is necessary”.
Mr Whitehead’s lawyers have argued the GP had a responsibility to further investigate the man’s symptoms after his colonoscopy and immediately after his positive bowel screening test result.
“We’re looking at a man who is dying, where arguably had the treatment been different in late 2017 or early 2018, he’d be on a very different course now and he likely wouldn’t be dying.”
The ABC contacted Mr Whitehead’s former GP but he was unavailable for an interview.
Tumour not ‘readily apparent’
Mr Whitehead also complained to the Australian Health Practitioner Regulation Agency (AHPRA) about his GP’s approach to his treatment.
The authority investigated the matter based on clinical notes and the guidelines from the time.
In its response to Mr Whitehead, the authority noted the GP’s observations that the case was “complex” and that the tumour was not “readily apparent” until the CT scan was performed in June 2018.
“He maintains that until that time, he was reassured by various sources nothing more sinister was responsible for the patient’s presentation,” the AHPRA response stated.
AHPRA closed the complaint, ruling the case was up to standard.
But Ms Robinson said that did not diminish Mr Whitehead’s argument for compensation.
“We are looking at a very different standard, we are looking at what’s known as a civil standard of care,” she said.
“We measure the GP’s behaviour by what other GPs say would be reasonable, based on their expertise and experience.
“We have expert evidence to indicate that despite what was done, more could have been done, and that as a result he’s suffering avoidable damage to his health.”
More focus on regional areas

Data released this month from the Victorian Cancer Registry reveals that survival rates for regional Victorians are consistently worse than in metropolitan areas.
Residents in metropolitan Melbourne have a 71 per cent chance of survival compared to regional Victoria’s rate of 67 per cent.
According to the most recent breakdown of smaller geographic areas from the Australian Institute of Health and Welfare, Maryborough had the worst cancer mortality rate in the state.
Cancer Council Victoria’s chief executive Todd Harper said there could be a number of reasons for that including poverty, smoking, and obesity rates, which are all higher in Maryborough.
“But it also might be related to the stage at which cancer is diagnosed. So, obviously, if the cancer is detected at an earlier stage there are much better prospects for a healthy recovery,” he said.
“It’s really important that we focus our prevention efforts, our treatment and supportive care efforts, in those areas to make sure that people in those areas have access to the best treatment that we know is available now.”
Source: ABC Ballarat By: Charlotte King
Support families fighting financial toxicity of cancer here