Advanced radiotherapy – at a fraction of the cost
EmpowerRT, a social enterprise company spun out from the University of North Carolina(UNC), has an impressive goal: to help resource-limited cancer clinics in developing countries improve radiotherapy, at just 5–10% of the cost of purchasing modern technology.
Currently, there is a huge disparity in cancer care across the world. About 70% of deaths from cancer occur in low- and middle-income countries (LMICs) and, according to the World Health Organization, it is these LMICs that will face the highest increase in cancer death rates in decades to come.
One underlying reason for this disparity is that many cancer clinics in LMICs still rely on older generation radiotherapy equipment, with no funds available to update to modern digital-based systems and the associated infrastructure. And while advances in radiation therapy technologies, such as the introduction of intensity-modulated radiotherapy (IMRT, which has been standard-of-care for years in developed nations), can improve tumour targeting and clinical outcomes, such systems are simply too expensive for many cancer clinics in LMICs.
“This is the really sad truth,” says EmpowerRT’s founder and president Sha Chang. “Many patients in developing countries die and suffer, not because the world doesn’t know how to treat their cancers, but because they have no access to the treatments. Our mission is to help people in low-resource countries to improve the quality of radiotherapy using existing resources, without spending millions of dollars that they don’t have.”
EmpowerRT is tackling this problem by offering a technology that enables any radiation delivery system to provide IMRT, using a low-cost compensator placed in front of the treatment beam. The compensator comprises a styrofoam mould filled with tungsten granules. It can be fabricated using a milling machine, assembled on site and, after treatment, the tungsten can be recycled to treat other patients. “The core belief of EmpowerRT is that we can advance cancer care by doing more with less, doing more with what is already available, and doing it simply”, says Sha.
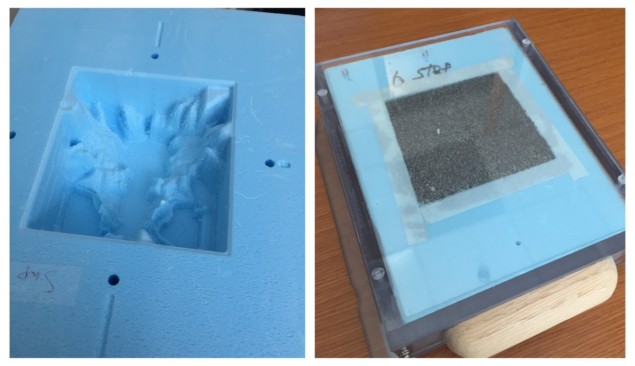
Similar to modern radiotherapy systems, the IMRT compensator shape is individually designed to attenuate the radiation beam to maximize dose to the tumour target while minimizing dose to nearby healthy tissue. “Using this approach, we can make existing radiation therapy machines in LMICs deliver a more advanced treatment. That’s the beauty of it,” says Sha. She explains that the recyclable compensator IMRT solution was developed at UNC before multileaf collimator (MLC)-based machines were widely available, and was used in treatments for 14 years and 1400 patients before UNC terminated its use after migrating to digital-based radiotherapy.
“We developed the recyclable compensator IMRT technology at a time when we were in a manual operating environment that’s still used in many low-resource settings. So we know this technology is feasible in that environment,” says Sha. “We want to give our proven technology a second life that can benefit more cancer patients.”
In addition to the recyclable compensator IMRT technology, EmpowerRT also offers treatment planning software and e-chart, a digital patient chart software designed for manually operated clinics. “Our goal is to bring the many benefits of a record and verify system to low-resourced clinics in LMICs,” says Sha. “We are also bringing in grid therapy, a novel therapy that benefits large and late-stage tumours, which are more prevalent in developing countries.”
The company also provides extensive training and support, to help sites introduce IMRT – everything from quality assurance and patient selection to setup – in order to establish an effective and safe treatment programme.
Inaugural installation
EmpowerRT has now installed this technology at its first site – the Cancer Diseases Hospital in Zambia. The country’s sole cancer hospital, it has three basic radiotherapy machines, none of which were previously able to deliver IMRT.
The EmpowerRT team offered remote training on the treatment planning software and also travelled to Zambia three times for extended onsite training and dry runs. Sha notes that the training focused on knowledge transfer: “we train the trainer, and then watch the trainer train others,” she explains.

“The training was excellent and the time spent was more than expected, with various hands-on and ‘real patient’ practice cases,” says Mulape Kanduza, chief medical physicist at the Cancer Diseases Hospital. “My first impression was ‘why is this renowned professor from UNC interested in working with our department?’. Effort was put both by the trainees and trainers and I believe the output is evident.”
Challenges such as machines breaking down and long delays in performing repairs, which are not uncommon in a LMIC environment, exacerbated by COVID-19-related travel restrictions, mean that the Cancer Diseases Hospital has not been able to complete an IMRT patient treatment yet. “But we have overcome many unexpected challenges, and the Zambia team of doctors, physicists and radiation therapy technologists all learned a great deal,” says Sha. “They are confident that they can do this new procedure independently, with us remotely doing the review and monitoring. That’s the success.”
“The future is very positive in that we have created a lasting relation to draw from,” Kanduza tells Physics World. “The positive outcome [will be] seeing an IMRT patient treatment being executed and knowing that the outcomes will be much better than treating with other conventional techniques.”
“Improved quality assurance in the workflow, using the Excel-based e-chart to review treatment records, has allowed us to think differently and to acknowledge change,” Kanduza adds. “One measurable outcome is that EmpowerRT’s e-chart system can work in a low-income setting such as ours.”
Looking ahead, EmpowerRT is now in talks with cancer clinics in Nigeria and Indonesia. The company is also partnering with organizations such as Clinton Health Access Initiative, which has worked for decades to reduce the burden of disease in LMICs, and Rayos Contra Cancer, which focuses on global radiotherapy training.
“We are also writing an NIH small business proposal targeted to feasible and effective cancer solutions in LMICs,” says Sha. “The next step is not only looking for where we can help, but how as a social enterprise company we can continue to grow, to partner with more like-minded global cancer care organizations and make a difference together.”
Source: PhysicsWorld By: Tami Freeman
Support families fighting financial toxicity of cancer – here.
